It started out with a ambulance ride to the emergency room. I was x-rayed, and then the doctor came by and said that I had broken my ankle in 2 places. It was not a compound fracture, so the next step would be to re-set the fracture. She the asked if I would like to be sedated for this procedure, or I could remain conscious, and endure a lot of pain. (I went for the sedation route). She brought a release form to sign, and mentioned that the type of sedation had some side effects like out of body experiences.
Week #1
I awoke from the procedure with a nurse laying on my lap, and holding my leg while a full length leg support cast with ace bandage was being wrapped up. After this I was given some pain pills, a set of crutches, some brief instructions on how to use them, and discharged, with a referral to get an appointment as soon as possible with an orthopedic surgeon.
The following day I got to the doctors office, and he came to see me for 5 minutes. He ordered the full length cast to be replaced with a half leg cast, so I could get around more easily. This was done without any pain relief, and was one of the most painful things I had endured so far. I was told that they would schedule surgery for the following week, an that I must keep down, my leg elevated, and keep it iced to reduce, and prevent any further swelling. If the swelling was not reduced by surgery time, It would be cancelled, and re-scheduled a week later. Some real incentive to follow the doctors orders. at the end of this week, I had to make a small field trip to the hospital for a pre-screening interview. This consisted of a blood pressure reading, a blood oxygen reading and a series of questions about history, and any nutritional supplements that I was taking. They give you a handout, that details exactly what you need to do the day of your visit, and how the events will unfold.
How to take a shower
1) Get a 5 gallon plastic bucket and place it upside down in the tub. Cover it with a hand towel.
2) Align a chair up next to the tub directly across from the bucket. Sit in the chair so that you un-injured leg is next to the tub.
3) Swing your un-injured leg into the tub, using your crutches if necessary, or other hand holds the may be in the tub, transfer yourself in and onto the bucket so you are seated. Leave your injured leg out resting on the chair, while you shower. Reverse the process to get out.
Week #2
Into the hospital at early AM, I was taken to a room and changed into a hospital gown, and an IV started I was visited by the anesthesiologist, the surgical nurse, who explained exactly what was in the operating room, and what would happen once we were in there and finally the doctor, who came in to examine my foot for swelling, he said all looked ok, and took a skin marker out and put a mark, on the foot and leg to be operated on. He said that was a required step. after that I was wheeled into the O-R and helped onto the table, just as the nurse had explained earlier. an oxygen mask was clapped onto my face, the anesthesiologist, looked around the room, and asked "Is everybody ready ?" (I was a trap team captain for several years, and this is the same line you ask the team before you start the round)
I awoke about half way from the O-R to the recovery room, sat straight up in the bed, and had the most pain that I had ever experienced in my entire life. The recovery room nurse started some type of intravenous pain medication, and told me that I was fighting it, I was not sure how I was doing this, but after about 20 minutes that pain was down to a manageable level. I was rigged up with a pushbutton pain medication machine, and it's operation was explained to me. after that I was pushed up to the hospital room. given a remote control pendent for calling the nurse bed adjustment and TV set control, and a machine that inflated and deflated a balloon every 15 seconds or so was attached to the sole of my other foot. It was explained that this was to prevent blood clots.
Week #3
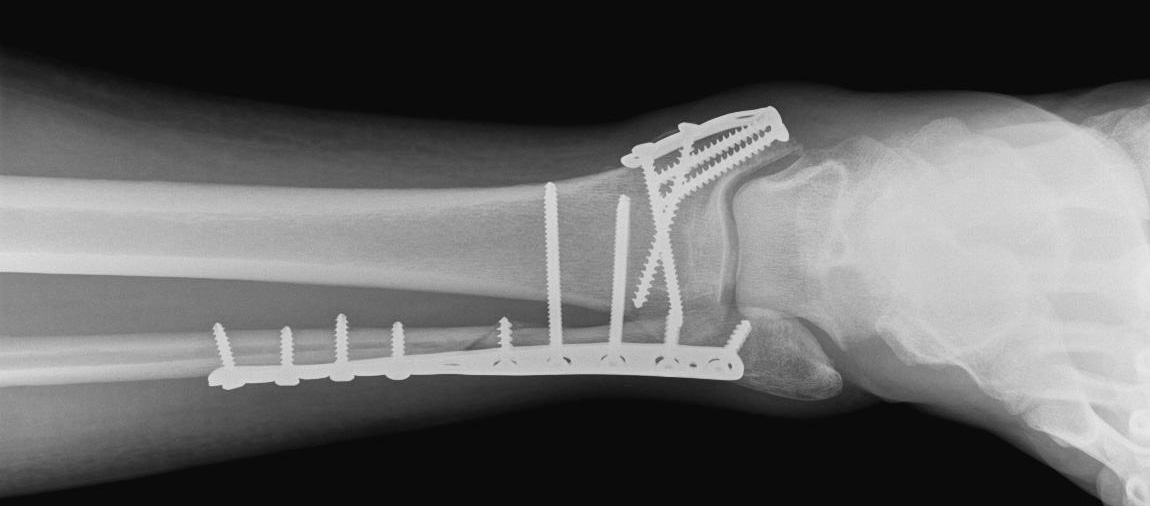
Return visit to the doctors office. This time I took the pain pills prior to the visit, expecting more cast work to be done. I was discharged from the hospital with a splint type cast on the back of my leg and leg secured with ACE bandages. At this visit it was removed, and I was sent down for an X-ray. On returning from the x-ray a nurse removed the stitches, (uncomfortable but not bad) put on super glue, and steri-tape. the cast technician came in and this time wrapped my leg in a cotton bandage, and then applied a more permanent type cast made of some type of fiberglass, and water activated resin. Prior to this he has you sit on the edge of the bed, and place your foot on an angle stand, and puts your foot at exactly 90 degree bend(It does not want to do this after 3 weeks of immobilization). I assume this is to get everything correctly lined up. I was told to make a return appointment in 4 weeks, and the same orders : Leg elevated stay down, keep it iced.
This 4 week wait was the most boring, I was cooped up in the house during the middle of summer, and by the end of the 4 weeks, the cast was highly irritating. The pan pills caused a lot of depression, so I found that ibuprofen worked just as well.
Week #7
Back to the doctors office. This time the cast was sawed off with a combo die grinder with cut-off wheel, and shop vac device. I was sent down to be x-rayed again, and upon returning noticed that my leg was about 60% of the size of my other leg. My leg was then wrapped up in an ACE bandage, and I was give a plastic boot that used velcro to secure your leg into it, and it also had a pump on it that inflated the liner to provide a snug fit for you leg. I was dismissed, and told to make an appointment with a physical therapist, and a follow up appointment in 4 weeks.The doctor said that I would be up and walking around by myself without crutches in 4 weeks. I am released to return to work the following full week
Week #8
Visit with physical therapist. I am shown how to put 25% of my weight on my surgical foot, and set up 2x week appointments. the routine that follows is such:
10 min on stationary bicycle
10 min on an elliptical board with a removable half ball of various sizes that allows you to rock you ankle in a 360 orbit but controls the amount of angle by the shape of the board, while hanging onto a rail
10 min on an inclined plane stepping on and off while hanging onto a rail
10 min on a platform with handrails putting various loads on my foot
10 min on a table, and the therapist stretching and pulling on the joint.
I am also given 2 large stretchy bands that allow you to pull and stretch you ankle joint at home. This routine goes on for 4 weeks, each week adding a 1/4 more of you body weight on the leg until full weight is achieved in 4 weeks. During this time you are only allowed to let water from the shower run down you surgical leg, no scrubbing at the incisions. You can however scrub everything else to remove 8 weeks of built up dead skin.
At 75% weight I am reduced to using only one crutch, and no longer use the inflatable plastic boot. at 100% weight load, I only use a cane for another 3 weeks to follow
Week #12
Check up visit with doctor, Re-x rayed, and told that everything looks fine. orders are to continue physical therapy for additional 4 weeks, and have a final checkup at that time. Physical therapy is still 2x per week and routine is modified to the following
10 min on stationary bicycle
5 min on an elliptical board with a removable half ball of various sizes that allows you to rock you ankle in a 360 orbit but controls the amount of angle by the shape of the board.
5 min stepping on and off of a 10" high step
10 min walking forwards and backwards on a 25' ruled line in the floor
10 min on a mat with a circle divided up into 1/8's and lunging forward or backward in sets at various angles
10 min on a bench weight machine leg pressing 1/2 my weight with only surgical leg, and 3/4 my weight with both legs
10 min on a table, and the therapist stretching and pulling on the joint.
This routine continues for another 4 weeks. at the end I am able to walk without much of a limp, and no cane.
Week #16
Final Doctor visit, and X-ray. At this visit I am told that I have bent 2 screws, and they will probably break at some point, but don't worry about it. If the screws become an issue in the future they can be removed, It would not be out patent treatment, and I would be laid up for another 3 to 4 weeks. Other than that I am discharged. Only issue I have at this point is the relentless swelling. I have bought support socks and wear one for the next 20 weeks.
Week #28
Its been quite a few months now, I take vigorous 1/2 hour walks at lunch with no side effects, about once a week I have some discomfort on the side of my leg with the long plate, I cant relate this to anything in particular. I have a general stiffness after being seated for more than 2 hours, and a mild limp for the first 20 or so steps until I get going. again. I will attempt to begin jogging in the next few weeks once the snow and Ice have gone.
I can still make it through the airport security devices even with all of this hardware in my leg
Update: I have had several email comments to this page, and feel that I should update it with more recent information. It's been tough to face up to it but I want everybody to know what may lie ahead.
6/2011
Week #35
The swelling in my ankle has never subsided. I continue vigorous walks, but I am not able to run, there seems to be no spring in my ankle, and every foot land is a hard impact, so running has been removed from my list of exercises I'm noticing some additional swelling on the inboard side of my ankle below the tibia bone. When sitting for a few hours I have a limp and pain for the first 20 or so steps
Week #40
The pain has subsided and I resume my walking routine
Week #50
The pain has gradually increased, and my walking is cut down to around a mile divided into 3 trips during the day
Week #60
Pain has increased to the point I can no longer walk without a limp, I give up walking as a form of exercise. I also must use a cane for the first 1/2 hour or so of mobility in the morning.
Week #70
I give in and make an appointment with the doctor, and an x-ray reveals that the 2 long screws between the tibia and fibula have broken off. There is also no spacing left between the joint in the ankle. Doctor's diagnosis: Osteo arthritis
It was explained that because of the nature of the injury, a high impact fracture that the cartilage can loose its blood supply just like a bruise, and not heal correctly. Also there is nothing that can be done aside from joint fusion. Don't even consider ankle replacement as an option, those joints are made for 90 pound 75 year old women.
I'm shocked and silent for a moment, the Doctor reminds me that no-one he has ever known has died from Arthritis.
I'm issued a large ankle brace, that immobilizes my ankle joint. I'm discharged in a state of shock, and forget to get another photo of my X-ray.
Week #80
I use the ankle brace daily for another 10 weeks. I was also given a prescription for Tramadol for sever pain and told to use and over the counter NSAID. There is some reduction in pain, I will not used NSAIDS as a routine daily medication. To date I have used 1/2 of a single Tramadol pill, otherwise a motrin or alieve pill for days where I have really beat up my ankle by being on my feet all day. I no longer use the ankle brace daily, as it makes walking and driving difficult. I have to use the cane in the first 1/2 hour of morning mobility.
Week #100
I'm now able to get around in the morning without the use of a cane. The pain has subsided, I have learned how to live with a bum ankle now. If my activities are to be very physical, I put on the ankle brace, and go for it. I'm just prepared to be in a lot of pain that evening, or the next day.
I generally walk with a noticeable limp, and the wear pattern on my shoes has changed as my left leg takes a lot of the load, and my right toe points outward allowing my foot to somewhat roll as my joint does not want to flex as much as it once did.
Summary:
I am in no way qualified to render any medical advice, but it’s possible my situation could have been much improved if I had been told to take it somewhat easy after my discharge. I returned to my normal everyday lunchtime vigorous walks immediately. I had even begun to try and jog some.
At my discharge on week #16 the X-ray was fine, I examined it very carefully then as I had found on the internet that arthritis is a common outcome of a broken joint, and I was concerned at that time.
It’s my belief that if I had been a lot more conservative with my use of my ankle for another 6 months to a year afterwards that the extent of the arthritis could have been minimized. You should quiz your doctor, on this and be insistent about how much exercise, and the type of activity.
I absolutely will not consider ankle fusion surgery. The notion of my foot being rigidly attached to my leg at a fixed 90 degree angle is abhorrent. I found the ankle brace that does the same thing to be debilitating enough, it's tough to use the accelerator pedal.
At some point I plan to return for a visit to a doctor who specializes in arthritis, and discuss the possibility of joint replacement surgery for the future. The STAR ankle from SBi has been FDA approved, and looks somewhat promising.
One last note for now. Arthritis is not a guaranteed outcome, I work with several other folks who have broken their ankles as well, and have no issues.